What are the different types of pessaries?
Pelvic organ prolapse (POP), also known as vaginal prolapse is when one or more of a woman’s pelvic organs slip down from their normal position.1 There are many treatments for POP, but a conservative option is vaginal pessaries. They are removable devices inserted into the vagina to support the pelvic floor and attempt to restore the prolapsed organs back to their normal positions.2
Pessaries are generally made of inert plastic or silicone to prevent odours or absorption of vaginal secretions and are available in a wide variety of shapes and sizes. This allows Health Care Professionals (HCPs) to choose the treatment option that is best suited to individual patients needs.3
This article will explore the various types of pessaries and their indications for use.
Who can use pessaries?
Vaginal pessaries can be broadly split into two categories: support and space-filling pessaries.2
Support pessaries
Support pessaries include ring or an incontinence dish with or without additional support and Shaatz pessaries and are usually used for milder prolapse. They’re designed to sit against the vaginal walls and elevate or lift the prolapsed tissue within the vagina.3
They are generally considered the first choice due to their ease of insertion and removal.4
Space-filling pessaries
Space-filling pessaries are generally reserved for more advanced prolapses5
and work by filling the space within the upper vagina.3
They are available in a wide array of shapes including Gellhorn, shelf, cube, donut and Inflatoball pessaries.5
If you would like to learn more about this topic, we have published a full article on the "different types of pessaries available".
Factors for determining pessary type recommendation
As HCPs have various types of pessaries to choose from, each with different indications for use, they must first assess the patient before deciding on the most appropriate type of pessary to recommend.
They should determine:
- The shape of the vagina
- The severity of the prolapse
- If the patient would like to self-manage
- If the patient wishes to commence or maintain sexual activity4
Types of prolapse and severity
To help determine the correct pessary, HCPs need to determine the severity of the condition. There are different types of prolapse, and it is possible to have more than one type at a time, but the four most common are:
- An anterior prolapse where the bladder bulges into the front wall of the vagina.
- A uterine prolapse when the womb bulges or hangs down into the vagina.
- A vaginal vault prolapse in which the top of the vagina sags down1 — this happens in some women who have had surgery to remove their womb.5
- A posterior wall prolapse where the bowel bulges forward into the back wall of the vagina.1
When it comes to determining the severity of the prolapse, classification occurs on a scale of stages 1–4, with 4 being the most severe.1 This classification is used to help HCPs determine the most suitable type of pessary.
You can find out more about prolapse types and grading by visiting our article on "What is prolapse?".
How are pessaries fitted?
Fitting pessaries comes down to trial and error to find the best shape and size for the anatomy and prolapse type, with various sizes or types possibly being tried before finding the most suitable one. The fitting may be slightly uncomfortable for patients, but the pessary should not cause any pain after being inserted. Once in situ, the patient will be asked to walk around for 15–20 minutes to ensure the pessary stays in place, is not uncomfortable and urine can still be passed. A different size may be needed if it falls out, is uncomfortable or has side affects like preventing urination.6
Self-management of pessaries
Some women choose to manage the removal, cleaning, inspection and reinsertion of the pessary themselves, whilst others choose to continue seeing their HCP to review their pessary.7
Some pessaries, such as ring, are appropriate for self-management as they are relatively easy to insert and remove,7 however, pessaries such as a cube or Inflatoball must be removed and cleaned each night, so are not suitable for women who are unable to or do not wish to self-manage their pessary.4
The different types of pessaries
Pessaries can be divided into two different categories: support pessaries and space-filling pessaries.8 Within these categories, there are different shapes and sizes of pessary, all serving slightly different purposes.
Support pessaries
Support pessaries include ring with or without support and Shaatz pessaries and are generally favoured for milder prolapses.
Ring pessary
Ring pessaries are silicone or PVC rings that either come with or without additional support. They are often considered the first option when HCPs are deciding the treatment of POP due to ease of insertion and removal,3 association with less vaginal discharge and irritation, and the ability for women to have sexual intercourse with the pessary in situ.8
They are generally suitable for less severe prolapses (stages 1 and 2) but can sometimes be used to successfully treat more advanced prolapses.3
Ring pessary with knob
Ring pessaries with a knob are designed for women with both pelvic organ prolapse and stress urinary incontinence (SUI). The knob adds additional width to the pessary which may affect the sizing but provides support to the bladder neck to reduce SUI.
The pessary is inserted like a standard ring but with the knob to one side. Once inside the vagina, the pessary is rotated so the knob sits behind the symphysis pubis4 (the joint between the left and right pelvic bones).
Ring pessary with support
For women with a more significant prolapse or those who feel as though the prolapse is bulging through the pessary, a ring pessary with support may be offered. These pessaries provide a flexible supporting membrane with drainage holes that prevent the uterus from falling through the centre of the ring.4
Interestingly, although ring pessaries are usually used to treat milder prolapse, a recent study exploring the treatment of more advanced prolapse with ring pessaries with support found that they had a high success rate and few complications. Older patients were more likely to prefer the ring pessary with support due to its convenient use.9
Shaatz pessary
Shaatz pessaries are a circular, flat plate with drainage holes usually made of soft silicone and are. They are similar to a space-filling pessary called a Gellhorn but have no stem. They are usually recommended for women who struggle to maintain a ring pessary due to a low or shallow pubic notch.4
Some women are able to self-manage this type of pessary as self-removal is possible, however, it is more difficult than with a ring pessary due to the surface of the device creating a suction effect.8 They are also able to remain sexually active due to a lack of a stem.8
Space-filling pessaries
Space-filling pessaries are generally reserved for more advanced prolapses and are available in a wide array of shapes including Gellhorn, shelf, cube and donut pessaries.3
Gellhorn
Gellhorn pessaries are a circular, flat plate, often considered in women with a more advanced prolapse or in need of additional support. It has a stem in the centre to stabilise it in the vagina whilst the cervix or vaginal vault rests behind the flat plate of the pessary. Most Gellhorns also have holes to facilitate fluid drainage and are usually made from a flexible silicone.4
They are sized in two ways. Firstly, as with a ring pessary the outer diameter of the plate must be determined to fit comfortably without slipping. Secondly, the vaginal length must be considered to determine the selection of a short or standard stem.4
Removal and insertion of Gellhorn pessaries is more challenging and therefore cannot be done by most patients.3 As a result, self-management and sexual intercourse is considerably more difficult. Generally, patients will attend reviews in a clinical setting every 3–6 months.4
Shelf pessary
These types of pessaries have a kidney-shaped plate for support with a curved stem in the centre to stabilise it in the vagina. They are usually reserved for women with a more advanced prolapse.4
As with the Gellhorn pessary, there are challenges with self-management and sexual activity and patients typically need to attend a review every 3–6 months.4

POPY™
POPY™ was the world’s first silicone shelf pessary and is a more flexible and comfortable option compared to other plastic shelf pessaries which are made of an acetyl copolymer.4
POPY™ is available in a range of sizes available in both short and standard stem to suit different anatomies. It offers several benefits for patients.

Donut pessary
Donut pessaries are made from a flexible silicone and are designed to provide support by occupying the vaginal space. They are typically used more in advanced prolapse cases.3
Due to the shape and size, these pessaries are more difficult to insert and
remove and cannot remain in situ during sexual intercourse, so are typically not recommended for self-management.8
Cube pessary
Cube pessaries are made of a soft silicone and have 6 concave sides which are designed to suction onto the surface of the vagina, providing an effective option for more advanced stages of prolapse, such as stages 3 and 4.3,8
Unlike other pessary types including Gellhorn and ring pessaries, cube pessaries cannot remain in situ as vaginal secretions can become trapped on the surface of the pessary, so they needs to be removed and cleaned nightly.3,8 They are therefore only suitable for patients with a good degree of manual dexterity.

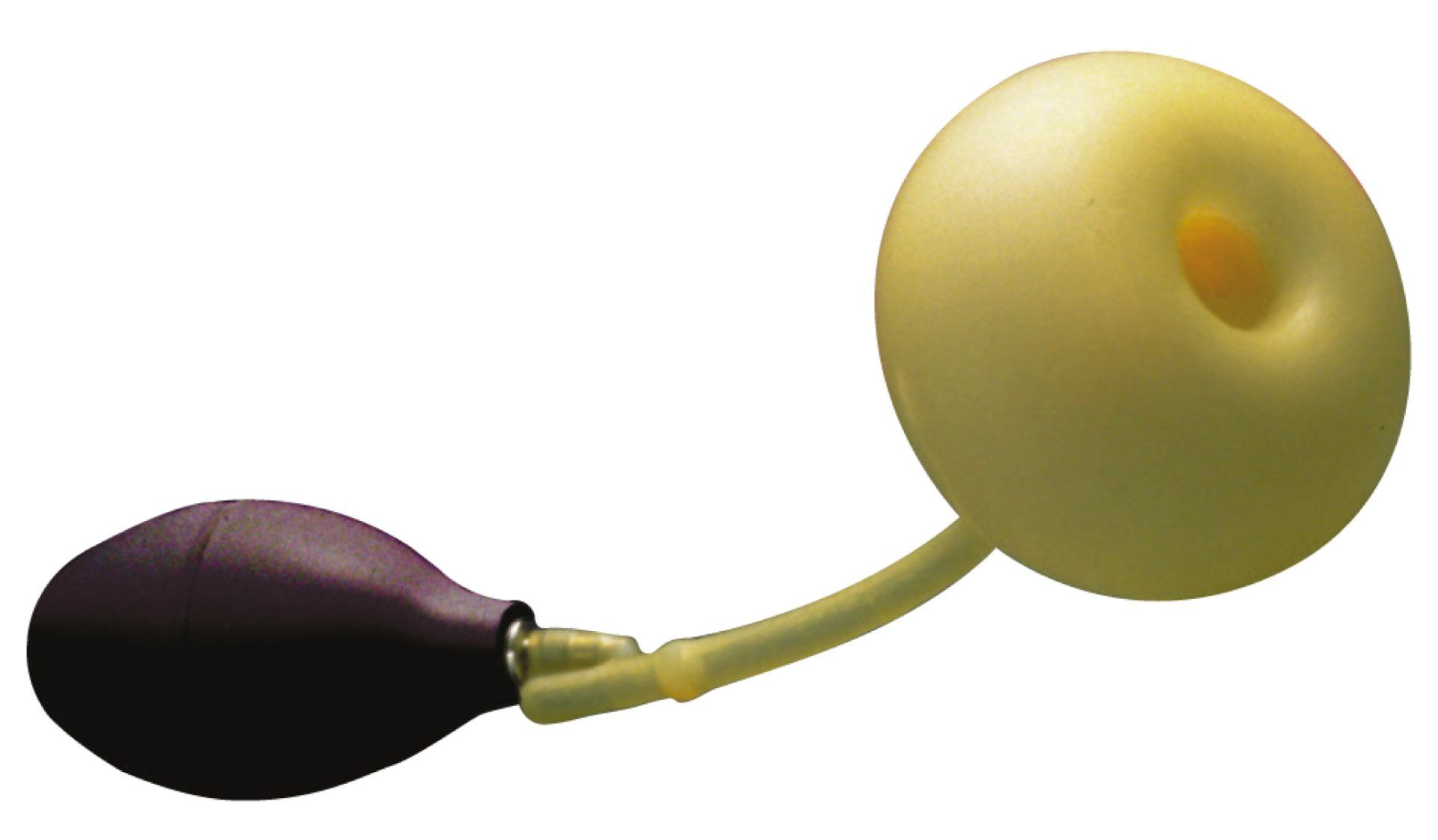
Inflatoball pessary
The Inflatoball pessary works similarly to the donut pessary by occupying space in the vagina but is inflated in situ.
It is made up of 3 parts. The head sits inside of the vagina and is inflated to provide support and deflated prior to removal. It is attached to the stem which sits out of the body and connects to the hand pump for inflation.
Insertion of these pessaries can be more comfortable for these patients as they don’t need to be inflated until in situ, however, they do need to be removed and cleaned nightly or prior to sexual intercourse, so are only suitable for women willing and able to self-manage.4
The Mediplus pessary range
Mediplus provides a range of pessaries to support POP, including both support pessaries and space-filling pessaries.
You can see our full range of pessaries by visiting our product page.
References:
- NHS. Pelvic organ prolapse. nhs.uk. Published March 24, 2021. Accessed February 8, 2023. https://www.nhs.uk/conditions/pelvic-organ-prolapse/
- Royal College of Obstetricians & Gynaecologists. Pelvic organ prolapse patient information leaflet. RCOG. Accessed February 8, 2023. https://www.rcog.org.uk/for-the-public/browse-all-patient-information-leaflets/pelvic-organ-prolapse-patient-information-leaflet/
- Jones KA, Harmanli O. Pessary Use in Pelvic Organ Prolapse and Urinary Incontinence.
- Commonly used pessary types – a practical guide. https://thepogp.co.uk/_userfiles/pages/files/pessary_types_guide.pdf
- Post-Hysterectomy Vaginal Vault Prolapse. RCOG. Accessed May 9, 2023. https://www.rcog.org.uk/guidance/browse-all-guidance/green-top-guidelines/post-hysterectomy-vaginal-vault-prolapse-green-top-guideline-no-46/
- White B. Vaginal pessary for prolapse. Published online June 2020. https://www.ouh.nhs.uk/patient-guide/leaflets/files/65609Ppessary.pdf
- Self management of vaginal ring pessary for pelvic organ prolapse. University Hospitals Sussex NHS Foundation Trust. Published November 16, 2022. Accessed May 9, 2023. https://www.uhsussex.nhs.uk/resources/self-management-of-vaginal-ring-pessary-for-pelvic-organ-prolapse/
- Thaker R. Pessaries for Treatment of Pelvic Organ Prolapse GLOWM. Published July 2014. Accessed February 8, 2023. http://www.glowm.com/section-view/heading/Pessaries for Treatment of Pelvic Organ Prolapse/item/805
- Ding J, Chen C, Song X chen, Zhang L, Deng M, Zhu L. Successful use of ring pessary with support for advanced pelvic organ prolapse. Int Urogynecol J. 2015;26(10):1517-1523. doi:10.1007/s00192-015-2738-1
Company REG. NO. 2051641
Copyright © 2020 Mediplus Ltd.